This article is part of the Under the Lens series

Intermountain Healthcare in Utah, along with several other groups, created the Utah Housing Preservation Fund to buy and preserve affordable units before they’re snapped up by for-profit developers. While plans continue, COVID-19 has changed things a bit. Photo by flickr user Ben P L, CC BY-SA 2.0
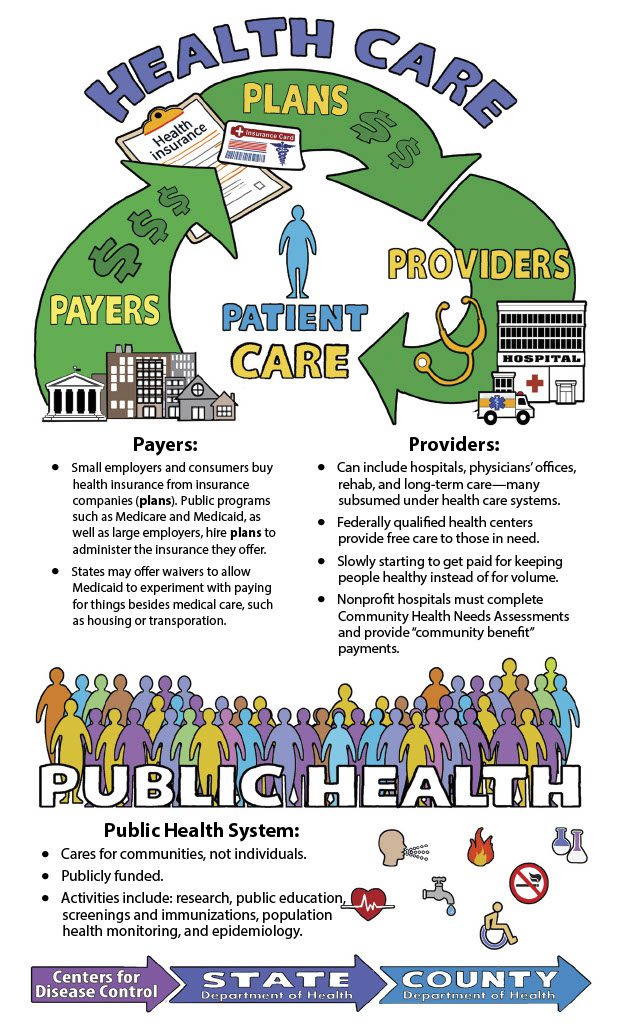
For health care institutions and community development organizations that focus on low-income communities’ social determinants of health, this year has been a doozy. The concept that a person’s health is deeply affected by their socioeconomic status, education, housing, and environment is a relatively new one, and many initiatives around the country designed to address those factors were just getting off the ground when the coronavirus pandemic began spreading last spring. Suddenly, hospitals and other health care institutions had to radically shift resources to treat a brand-new illness. Patients and doctors alike canceled elective procedures, vastly reducing hospital revenues.
At the same time, though, low-income communities and people of color have been disproportionately hard-hit by the virus, laying bare the exact inequities these programs have been aiming to address. And the racial justice protests that first erupted this summer after George Floyd’s killing by police have further underscored the depth of structural inequalities in this country.
As a result, while some programs have been put on hold or seen their funding reduced, most of the health care and community development leaders spearheading them have only become more passionate and determined.
“There seems to be a collective consciousness about getting at the deep roots of poverty and how to combat it, in the space of racial equities,” says Colleen Flynn, director of national programs at Build Healthy Places Network, which brings together community development groups and health care organizations. As her organization wrote in a recent article, “Community development and the health care sectors no longer have to convince people that health is a byproduct of our social and physical environments. COVID-19 has made that abundantly clear.
But programs’ outcomes have been very differently affected by the crisis, with initiatives responding to varied pressures. And while COVID-19’s impact has mostly resulted in limits on program activities, advocates say it’s also opening new possibilities and avenues for action.
Staying Strong and Committed
At the Center for Community Investment (CCI), which is running an ambitious program mentoring a handful of large health systems to bolster their affordable housing efforts, “no one’s pulled out,” says Robin Hacke, executive director. “Every single team has continued working. [In some cases] hospitals have assigned someone more senior to keep the work going. It’s been very surprising.”
Hacke says that while funding has declined in some cases—“if investments were in the three-digit millions, maybe they’re now in the two-digit millions”—the health care leaders are even more determined to get the work done right. At a recent meeting, CCI provided trainers upon request who could help participants examine their efforts through a racial equity lens and better identify the root causes of communities’ health discrepancies.
David Zuckerman, director of the Healthcare Anchor Network, had similar observations. In June, the network, which includes 52 health systems focused on investing in upstream determinants of health, held its bi-annual convening online; it had 450 unique participants, three times the usual number. Participants were hungry to talk about health disparities, and a session on racial equity was particularly popular.
“We haven’t seen any drop-off in participation; in fact, we have several new members,” says Zuckerman.
Still, that comes with a caveat. To be able to do this work, institutions need committed resources in the form of people and funding. And both of those can be limited at a time when staff are being furloughed, leaders’ attention is elsewhere, and revenues are down.
That points to the fact that the institutions most able to continue this work are the ones that built their community engagement infrastructure long before COVID-19 struck.
“It’s harder to do this within a crisis,” says Zuckerman. “If you didn’t already have positions resourced and internal conversations about hiring process or advocacy strategy—those are all very difficult to move forward with while in a crisis.”
LISC as a Forerunner
In discussions about systems that haven’t retreated from their commitments, Kaiser Permanente and its recent partnership with Local Initiatives Support Corporation (LISC) come up repeatedly. In June, the two organizations announced that they would each commit $30 million in capital for loans to minority-owned businesses; companies across eight states where Kaiser operates will be able to access loans of $100,000 to $4 million.
“It’s significant for several reasons,” says Julia Ryan, LISC’s vice president for health initiatives. First, she explained, this initiative focuses on economic opportunity, not just affordable housing. “The housing-health connection is well researched, but the job-health connection is less well documented.” So for Kaiser to be saying, ‘We get this’ is a big deal, Ryan explains.
The timing has also turned out to be critical, says Ryan. Kaiser and LISC began working on this concept well before the coronavirus and subsequent recession, but hustled to make sure they could get it in place in time to help the many Black and Brown-owned businesses that have been struggling during this uncertain time. The loans can be used to help companies recover from the virus’s impact, to strengthen their ability to offer quality jobs, or to transform underutilized commercial corridors.
The collaboration with Kaiser is one of several of LISC’s partnerships with health care institutions that are now bearing fruit. Last fall Sentara, a Virginia-based health care system, announced it would provide $40 million in loans and another $10 million in grants to LISC for affordable housing in the state. That’s still on track, too, and especially useful during the pandemic. “Everything about community development has gotten harder; we need cheap money to get high impact projects done,” says Ryan.
Ryan acknowledges that LISC is currently particularly well positioned to partner with health care groups. “In the last several years, we’ve embraced the social determinants of health. We’ve always looked at this through a racial equity lens, but now we’re trying to be even more thoughtful,” she says. “And there’s now a lot of appetite for strategic collaboration with CDFIs” like LISC.
The organization is also examining new avenues that have opened up in recent months. Far fewer medical procedures have been scheduled because of the coronavirus, which means that insurance companies around the country are flush with revenues; in the second quarter of 2020, some earned double the revenues they took in a year before. Could they be enticed to provide some of the capital that’s disappeared since March? LISC and other groups have been looking into it.
At the end of September, LISC announced a new housing fund in Arizona that includes significant investments from the insurance companies United Healthcare and Aetna, as well as grant funding from seven managed-care organizations. While the details were hammered out prior to COVID-19, the fund could serve as template for other partnerships with health plans.
Finding Creative Ways to Keep the Work Going
Intermountain Healthcare is another institution that has no plans to retreat from its commitments. The giant Utah-based health system has had big dreams: together with the Clark and Christine Ivory Foundation, Zion Bank, and Utah Nonprofit Housing Corporation, it created the Utah Housing Preservation Fund to buy and preserve affordable units before they’re snapped up by for-profit developers in Utah’s supercharged housing market. The $20 million fund, which includes $4 million from Intermountain, made its first purchase—24 duplexes—in March.
So far, so good. In fact, the project has been working so well, and the need is so great, that Intermountain and its partners raised their goal for the housing fund to $100 million. The fund’s formula would remain the same: 20 percent would come from Intermountain’s impact investment funds, 10 to 15 percent would be grants, and the rest would be in the form of traditional debt.
But COVID-19 has changed things a bit. “Our strategy was to find grant dollars and the rest will follow. But the folks we were working with locally put a hold on grants,” says Nicholas Fritz, director of impact investing at Intermountain. That’s created some hurdles for the project’s $100 million ambitions.
Nonetheless, says Fritz, the pandemic has created a new sense of urgency. And some new possibilities. When eviction moratoriums end, many distressed properties may come on the market. So even in the absence of new fundraising and commitments, says Fritz, “maybe there will be some coming opportunities to make sure these remain affordable.”
To better respond, Intermountain and its partners are rethinking the fund’s structure. For example, could it be useful to establish a two-phased approach that would allow them to use the funding up front to buy real estate, while determining a permanent financing structure later? That might help the housing fund better compete with institutional investors like the Blackstone Group, which often has the advantage of being able to pay for properties in cash. “We’re trying to be in a position to take this on,” says Fritz.
In Ohio, Nationwide Children’s Hospital is also looking for creative ways to continue doing its work. The hospital has been a leader in its work of building, renovating, and repairing affordable homes in Columbus, spending $32 million to build or rehabilitate 375 homes in the Columbus area since 2008. But one of its key funding partners has been the city—which is currently putting everything it has into helping residents directly.
“They can’t commit time or dollars beyond what was already committed,” says Kelly Kelleher, a pediatrician and the vice president of community health at Nationwide. “Their inability to focus on this means we’ll interrupt this building phase we were in.”
In response, Nationwide, like LISC, has been eyeing health plans as potential partners. “We’re trying to get managed care organizations to step in and do something: that’s the goal,” says Kelleher. Currently his system has asked one of the managed care organizations to come in on a deal with very low-interest rates.
“It’s nice: it’s a new partner, and it’s a good deal that they’ll commit,” says Kelleher. But it’s not a full substitute for the grant and equity money the city was supplying that needs to lie at the base of an affordable housing capital stack.
Kelleher is also wondering if the pandemic could simultaneously result in more opportunities to create housing. “People are switching from face to face [visits] to telemedicine, and that might continue, because people are so much happier,” he says, echoing analysts around the country. Kelleher explained that patients have expressed satisfaction with waiting at home for provider visits, rather having to secure child care and transportation in order to sit in crowded waiting rooms.
Less room needed for patient visits would result in a shrinking of health care institutions’ giant footprint. At Nationwide, no decisions have been made about what to do with all that property, but administrators are already thinking about it. Could some of that space be converted to affordable housing instead?
Residents Need to be Deeply Represented
Health care institutions are only one side of these partnerships, though. On the other side are community development organizations that are facing their own challenges. For many of these groups, funding is perennially limited, and seeing projects halted is a manageable disappointment.
But housing groups and other nonprofits working in this field are often based in communities of color, many of which are struggling profoundly from the effects of the coronavirus. Not only have they fallen sick at disproportionate rates; Black and Latinx employees make up a large share of the essential workforce and are forced to leave home regularly, often without child care. Others may have simply lost their jobs and sources of income. Hands down, these are the demographics hit the hardest by the crisis.
For some of these groups, their partnerships with health care systems and their already-in-place networks have been a boon. Others, though, have felt themselves shunted to last place by health providers when it comes to care and assistance—an experience that feels reminiscent of many other times.
In Montana, for example, Common Good Missoula—a coalition of about 40 community organizations—hired several full- and part-time community organizers last fall. The goal then was simply to help low-income Missoula residents better access health care, food, and housing.
The organizers had about six months to settle into their jobs before everything shut down due to the pandemic. That turned out to be just enough time for them to get up to speed. “The fact that we had the relationships in place and were having dialogues, we were very much able to rapidly transition our organizing work from the long game to the short game of ‘what do people need right now, what are they experiencing, what kind of mutual aid can we help with, and how can the health department and Partnership [Health Center] pivot to be more responsive to what people are experiencing right now,’” says Hallie Carde, one of the organizers.
The organizers—with the help of several of the health-related groups in the coalition—contacted hundreds of residents to hear their experiences and identify themes. From there, they were able to report those needs to elected officials, who used the information to craft assistance policies that the organizers were later able to gut-check with residents. It’s a feedback loop that worked largely because it was in place prior to COVID-19, and because residents were able to directly voice their needs.
Low-income residents of Greensboro, North Carolina, weren’t quite so lucky. Josie Williams heads the Greensboro Housing Coalition, an organization that spearheaded a multi-stakeholder health-related collaboration in a low-income area of the city. That project is now part of the national Invest Health initiative and includes partners like Cone Health and the county health department, which has been working with the community for several years.
But although the coronavirus became critical in March, free mobile testing wasn’t available in that Greensboro neighborhood for several months. “And that’s when it was needed the most,” says Williams. “In the midst of something like this, you should be prioritizing your recovery resources according to the clear data pointing to these areas that are already marginalized, disenfranchised, and at higher risk.”
When Williams pointed the discrepancy out to health providers, she says, “I literally heard an ‘aha’ moment—a sentiment like, ‘Wow, I didn’t think all these [low-income] people would come out.’ That just shows to me a lack of understanding regarding disparate impact.” In other words, when the rubber hit the road, those health care providers weren’t ready to put into practice some of the learning they’ve done around inequities and the social determinants of health.
But Williams says she does see Cone Health as a genuine partner, and many of the people focused on community health there feel like real allies. When low-income Greensboro communities needed help accessing food last spring, it was Cone Health that helped start a food distribution program that eventually took off, serving 100 meals a day at six sites and led by volunteers from the community.
It worked, though, not simply because of Cone Health’s involvement, but because of all the organizations and people who contributed to it. “It didn’t come out of any one organization; it’s a testament to the power of grassroots organizing in the midst of all of this,” says Williams.
|
|



Comments