
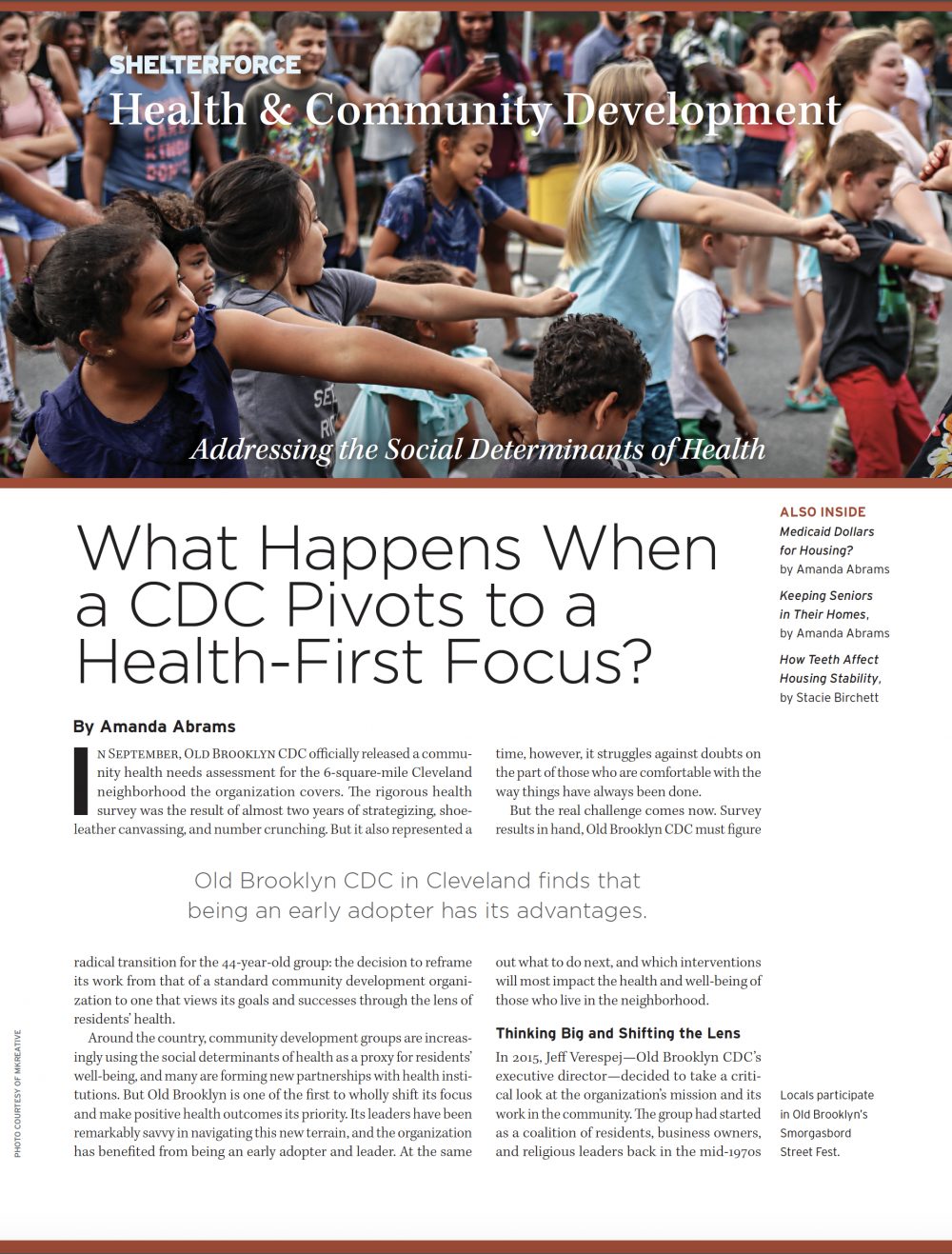
Ellen Gagne leads a group activity on creating winter bird feeders using a bagel, peanut butter, and birdseed. Photo by Karen Pike
Most senior citizens want to stay in their homes as they age, but health considerations often make that impossible. Almost a decade ago, Vermont’s Cathedral Square Corporation, which has been building affordable senior housing for 40 years, questioned the seeming inevitability of that pattern. Could its staff design a slate of health interventions that would address older residents’ physical and emotional needs and also allow them to grow old at home?
The result is Support and Services at Home (SASH), a hands-on program that does just that. Operating across the state of Vermont, SASH promotes the coordination of health care by connecting elderly residents with community-based services and a traveling wellness nurse. The program allows residents to continue living as independently as possible, and—as a team of researchers recently wrote in HUD’s Cityscape journal—it makes a significant dent in health care costs, as well.
But it’s only possible because of the real application of concepts many organizations only give lip service to: partnership, collaboration, and connecting people. Those elements were integral from the start, and remain key to its success.
Cathedral Square developed the concept of SASH in 2009. Working with about 60 older adult residents at one of the organization’s housing sites in Burlington, Cathedral Square’s staff designed the program by querying experts: the people themselves.
“That was very intentional: we knew that they were probably the ones with the answers about how to build a system,” says Molly Dugan, the director of SASH. “We really worked with them; we had weekly meetings with residents and their families or guardians where we’d choose a particular topic”—say, issues around coming home from a hospital visit—“and we heard a lot about what was working well, what wasn’t.” Existing community partners who work with seniors, such as home health agencies and departments of aging, were also part of the discussions.
Starting in 2009, Cathedral Square piloted the program for a year. In 2010, SASH joined the state’s health care reform initiative—Vermont Blueprint for Health—in an application to the Centers for Medicare and Medicaid Services for one of its innovative payment reform demonstration programs. Funding through that program was secured in 2011 and allowed for Medicare funds to be used differently and provide payments for primary prevention efforts, including those prioritized by the SASH program.
Today, the program is in all of Vermont’s 14 counties and helps roughly 5,000 older residents, most of whom live in low-income housing developments. SASH has divided the Vermont map into six geographic areas, and they’re all administered by affordable housing providers, including Cathedral Square. That’s crucial, says Dugan: “Those organizations have the connections with their people and communities,” which means they’re better able to identify residents’ particular needs and habits.
A full-time care coordinator and a part-time nurse visit the residents regularly, but a big part of their roles is to connect the residents with services that can help them. Those service providers—from senior transportation agencies to grief support groups to healthy eating specialists—sign an agreement to collaborate with SASH staff and regularly attend meetings. “We’ve got to get services to where people live, and this simplifies it a whole lot,” said Dugan. “The existing organizations have years of experience, and they’re key.”
The wellness nurse, meanwhile, is in close communication with primary care providers. “[The nurses] are seeing their patients and have a lot of interesting information—for instance, ‘Here’s what’s really in the medicine cabinets of your patients,’ or ‘They’re really not using their walker like you told them to,’” explains Dugan.

SASH participants join in a weekly “Bone Builders” class in the community room at Town Center, an affordable-housing residence in Essex, Vermont.
Photo by Karen Pike
The upshot is that the participating seniors are happy. Dugan says she sees it every day, in the grateful letters she gets from residents’ family members and the small ways SASH staff are able to improve the seniors’ health and lessen their social isolation. “Our staff are charged with building trusting relationships,” says Dugan. “That is, what makes this participant tick? What do they need to stay happy and healthy? I know we’re making a difference.’”
And it’s a difference that’s quantifiable, as recently demonstrated by researchers from RTI, LeadingAge, and other organizations, who wrote about SASH in Cityscape’s November issue.
Their findings initially look disappointing: the study found that SASH has no significant impact on total Medicare expenditures. But the finer print is heartening. In fact, the programs administered by Cathedral Square, and other programs that specifically focused on urban areas, did show statistically significant savings, particularly in emergency room and specialist visits, two high-cost areas. In total, the programs administered by Cathedral Square saved $91 per beneficiary per month in Medicare dollars, while the urban programs saved $122.
Those numbers aren’t too surprising: Cathedral Square had run its SASH program for a longer time than the others, and utilized a team leader who was able to take over some administrative tasks and free up other staff members. And the urban programs allowed staff members to spend less time in transit and concentrate more closely on residents.
And that’s very meaningful, says Amy Kandilov, a senior research economist with RTI and the study’s lead researcher. “A lot of programs get tried and don’t show any effect at all. This is the glass half full: it has favorable results and we can see characteristics that will help move it forward.”
Robyn Stone, another member of the research team, and senior vice president of research at LeadingAge, the national association of aging-related nonprofits, agreed. “I think it was a fairly strong finding for urban areas, and the applicability is to most housing across the country, so it’s quite valuable. Also, it’s a consistent finding over multiple years,” she says, adding that those elements add real legitimacy to the program.
In fact, organizations in several other states have shown interest, and some are already implementing SASH look-alikes. Cathedral Square is working with a housing group in Minnesota to replicate SASH at five housing communities there. And the model is already being used in Rhode Island, in a high rise for low-income seniors in downtown Providence. Those residents are mostly Spanish speaking, and Dugan says, “It’s so cool to see such a different context and see the SASH model flourish there.


Comments